Abstract
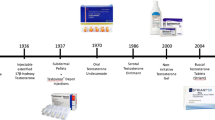
As there are limitations to current methods of male contraception, research has been undertaken to develop hormonal contraceptives for men, analogous to the methods for women based on estrogen and progestogens. When testosterone is administered to a man, it functions as a contraceptive by suppressing the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland. Since these hormones are the main stimulatory signals for spermatogenesis, low levels of LH and FSH markedly impair sperm production. After 3–4 months of testosterone treatment, 60–70% of men no longer have sperm in their ejaculate, and most other men exhibit markedly diminished sperm counts. Male hormonal contraception is well tolerated, free of serious adverse side effects, and 95% effective in the prevention of pregnancy. Importantly, male hormonal contraception is reversible, with sperm counts usually recovering within 4 months of the discontinuation of hormone treatment. Because exogenous testosterone administration alone does not completely suppress sperm production in all men, researchers have combined testosterone with second agents, such as progestogens or gonadotropin-releasing-hormone antagonists, to further suppress secretion of LH and FSH and improve suppression of spermatogenesis. Recent trials have used combinations of long-acting injectable or implantable forms of testosterone with progestogens, which can be administered orally, by injection or by a long-acting implant. Such combinations suppress spermatogenesis to zero without severe side effects in 80–90% of men, with near-complete suppression in the remainder of individuals. One of these testosterone and progestogen combination regimens might soon bring the promise of male hormonal contraception to fruition.
Key Points
-
The administration of exogenous testosterone and progestogens results in suppression of sperm production that might allow their use in a male contraceptive
-
The tolerability and side-effect profiles of these regimens are favorable
-
Such regimens are currently 95% effective at pregnancy prevention
-
Improved potency and methods of drug delivery might allow for the introduction of such a hormonally based male contraceptive in the next 10 years
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Anonymous (1999) Notice to readers: world's population to reach six billion. Morb Mortal Wkly Rep 48: 859
Henshaw SK (1998) Unintended pregnancy in the US. Fam Plann Perspect 30: 24–29
Besculides M and Laraque F (2004) Unintended pregnancy among the urban poor. J Urban Health 81: 340–348
Piccinino LJ and Mosher WD (1998) Trends in contraceptive use in the United States: 1982–1995. Fam Plan Perspect 30: 4–10
Martin CW et al. (2000) Potential impact of hormonal male contraception: cross-cultural implications for development of novel male preparations. Human Reprod 15: 637–645
Heinemann K et al. (2005) Attitudes toward male fertility control: results of a multinational survey on four continents. Hum Reprod 20: 549–556
Glasier AF et al. (2000) Would women trust their partners to use a male pill? Human Reprod 15: 646–649
Heckel MJ (1939) Production of oligospermia in a man by the use of testosterone propionate. Proc Soc Exp Biol Med 40: 658–659
World Health Organization Task Force on Methods for the Regulation of Male Fertility (1990) Contraceptive efficacy of testosterone-induced azoospermia in normal men. Lancet 336: 995–999
Handelsman DJ et al. (1995) Factors in nonuniform induction of azoospermia by testosterone enanthate in normal men. Fertil Steril 63: 125–133
World Health Organization Task Force on Methods for the Regulation of Male Fertility (1996) Contraceptive efficacy of testosterone-induced azoospermia and oligozoospermia in normal men. Fertil Steril 65: 821–829
Gu Y-Q et al. (2003) A multicenter contraceptive efficacy study of injectable testosterone undecanoate in healthy Chinese men. J Clin Endocrinol Metab 88: 562–568
Turner L et al. (2003) Contraceptive efficacy of a depot progestin and androgen combination in men. J Clin Endocrinol Metab 88: 4659–4667
Nieschlag E et al. (2003) Sixth summit meeting consensus: recommendations for regulatory approval for hormonal male contraception. Int J Androl 25: 375
Bagatell CJ et al. (1994) Metabolic and behavioral effects of high-dose, exogenous testosterone in healthy men. J Clin Endocrinol Metab 79: 561–567
Meriggiola MC et al. (1995) Testosterone enanthate at the dose 200 mg/week decreases HDL-cholesterol levels in healthy men. Int J Androl 18: 237–242
Zitzmann M et al. (2002) Contraceptive steroids influence the hemostatic activation state in healthy men. J Androl 23: 503–511
Sjögren B and Gottlieb C (2001) Testosterone for male contraception during one year: attitudes, well-being and quality of sex life. Contraception 64: 59–65
Ringheim K (1995) Evidence for the acceptability of an injectable hormonal method for men. Fam Plann Perspect 27: 123–128
Coert A et al. (1975) The pharmacology and metabolism of testosterone undecanoate (TU), a new orally active androgen. Acta Endocrinol (Copenh) 79: 789–800
Zhang GY et al. (1998) A pharmacokinetic study of injectable testosterone undecanoate in hypogonadal men. J Androl 19: 761–768
Behre AM et al. (1999) Intramuscular injection of testosterone undecanoate for the treatment of male hypogonadism: phase I studies. Eur J Endrocrinol 140: 414–419
Zhang GY et al. (1999) Injectable testosterone undecanoate for contraception in Chinese men. J Clin Endocrinol Metab 84: 3642–3647
Kamischke A et al. (2000) Intramuscular testosterone undecanoate with or without oral levonorgestrel: a randomized placebo-controlled feasibility study for male contraception. Clinical Endocrinol 53: 43–52
Kamischke A et al. (2001) Intramuscular testosterone undecanoate and norethisterone enanthate in a clinical trial for male contraception. J Clin Endocrinol Metab 86: 303–309
Junaidi A et al. (2005) Norethisterone enanthate has neither a direct effect on the testis nor on the epididymis: a study in adult male cynomolgus monkeys (Macaca fascicularis). Eur J Endocrinol 152: 655–661
Schearer SB et al. (1978) Hormonal contraception for men. Int J Androl 2: 680–695
Fotherby K et al. (1972) Effect of low doses of synthetic progestagens on testicular function. Int J Fertil 17: 113–119
Barfield A et al. (1977) Pregnancies associated with sperm concentrations below 10 million/ml in clinical studies of a potential male contraceptive method, monthly depot medroxyprogesterone acetate and testosterone esters. Contraception 20: 121–127
Bebb RA et al. (1996) Combined administration of levonorgestrel and testosterone induces more rapid and effective suppression of spermatogenesis than testosterone alone: a promising male contraceptive approach. J Clin Endocrinol Metab 81: 757–762
Anawalt BD et al. (1999) A lower dosage levonorgestrel and testosterone combination effectively suppresses spermatogenesis and circulating gonadotropin levels with fewer metabolic effects than higher dosage combinations. J Androl 20: 407–414
Anawalt BD et al. (2005) Very low-dosage oral levonorgestrel plus intramuscular testosterone enanthate suppresses spermatogenesis without causing weight gain in normal young men: a randomized clinical trial. J Androl 26: 405–413
Gui YL et al. (2004) Male hormonal contraception: suppression of spermatogenesis by injectable testosterone undecanoate alone or with levonorgestrel implants in Chinese men. J Androl 25: 720–727
Wu FC et al. (1999) Oral progestogen combined with testosterone as a potential male contraceptive: additive effects between desogestrel and testosterone enanthate in suppression of spermatogenesis, pituitary–testicular axis, and lipid metabolism. J Clin Endocrinol Metab 84: 112–122
Anawalt BD et al. (2000) Desogestrel plus testosterone effectively suppresses spermatogenesis but also causes modest weight gain and high-density lipoprotein suppression. Fertil Steril 74: 707–714
Kinniburgh D et al. (2002) Oral desogestrel with testosterone pellets induces consistent suppression of spermatogenesis to azoospermia in both Caucasian and Chinese men. Hum Reprod 17: 1490–1501
Anderson RA et al. (2002) Investigation of hormonal male contraception in African men: suppression of spermatogenesis by oral desogestrel with depot testosterone. Hum Reprod 17: 2869–2877
Hay CJ et al. (2005) A multicenter phase IIb study of a novel combination of intramuscular androgen (testosterone decanoate) and oral progestogen (etonogestrel) for male hormonal contraception. J Clin Endocrinol Metab 90: 2042–2049
Anderson RA et al. (2002) Suppression of spermatogenesis by etonogestrel implants with depot testosterone: potential for long-acting male contraception. J Clin Endocrinol Metab 87: 3640–3649
Brady DM et al. A multi-centre study investigating subcutaneous etonogestrel implants with injectable testosterone decanoate as a potential long-acting male contraceptive. Hum Reprod, in press
Neumann F and Topert M (1986) Pharmacology of antiandrogens. J Steroid Biochem 25: 885–895
Meriggiola MC et al. (1996) A combined regimen of cyproterone acetate and testosterone enanthate as a potentially highly effective male contraceptive. J Clin Endocrinol Metab 81: 3018–3023
Meriggiola MC et al. (1998) Low dose of cyproterone acetate and testosterone enanthate for contraception in men. Hum Reprod 13: 1225–1229
Meriggiola MC et al. (1997) An oral regimen of cyproterone acetate and testosterone for spermatogenic suppression in men. Fertil Steril 68: 844–850
Meriggiola MC et al. (2002) Twenty-one day administration of dienogest reversibly suppresses gonadotropins and testosterone in normal men. J Clin Endocrinol Metab 87: 2107–2113
Kamischke A et al. (2000) Potential of norethisterone enanthate for male contraception: pharmacokinetics and suppression of pituitary and gonadal function. Clin Endocrinol (Oxf) 53: 351–358
Kamischke A et al. (2001) Intramuscular testosterone undecanoate and norethisterone enanthate in a clinical trial for male contraception. J Clin Endocrinol Metab 86: 303–309
Meriggiola MC et al. (2005) Norethisterone enanthate plus testosterone undecanoate for male contraception: effects of various injection intervals of spermatogenesis, reproductive hormones, testis and prostate. J Clin Endocrinol Metab 90: 2005–2014
Kamischke A et al. (2002) An effective hormonal male contraceptive using testosterone undecanoate with oral or injectable norethisterone preparations. J Clin Endocrinol Metab 87: 530–539
Gu YQ et al. (2004) Male hormonal contraception: effects of injections of testosterone undecanoate and depot medroxyprogesterone acetate at eight-week intervals in Chinese men. J Clin Endocrinol Metab 89: 2254–2262
Pavlou SN et al. (1991) Combined administration of a gonadotropin-releasing hormone antagonist and testosterone in men induces reversible azoospermia without loss of libido. J Clin Endocrinol Metab 73: 1360–1369
Tom L et al. (1992) Induction of azoospermia in normal men with combined Nal–Glu gonadotropin-releasing hormone and testosterone enanthate. J Clin Endocrinol Metab 75: 476–483
Bagatell CJ et al. (1993) Comparison of a gonadotropin releasing-hormone antagonist plus testosterone (T) versus T alone as potential male contraceptive regimens. J Clin Endocrinol Metab 77: 427–432
Swerdloff RS et al. (1998) Suppression of spermatogenesis in man induced by Nal–Glu gonadotropin releasing hormone antagonist and testosterone enanthate (TE) is maintained by TE alone. J Clin Endocrinol Metab 83: 3527–3533
Behre HM et al. (2001) Suppression of spermatogenesis to azoospermia by combined administration of GnRH antagonist and 19-nortestosterone cannot be maintained by this non-aromatizable androgen alone. Hum Reprod 16: 2570–2577
Tomera K et al. (2001) The gonadotropin-releasing hormone antagonist abarelix depot versus luteinizing hormone releasing hormone agonists leuprolide or goserelin: initial results of endocrinological and biochemical efficacies in patients with prostate cancer. J Urol 165: 1585–1589
Herbst KL et al. (2004) Acyline, a gonadotropin releasing-hormone antagonist suppresses gonadotropins and testosterone for 15 days after a single dose. J Clin Endocrinol Metab 89: 5959–5965
Matthiesson KL et al. (2005) Novel male hormonal contraceptive combinations: the hormonal and spermatogenic effects of testosterone and levonorgestrel combined with a 5-α-reductase inhibitor or GnRH antagonist. J Clin Endocrinol Metab 90: 91–97
Cho N et al. (1998) Discovery of a novel, potent and orally active nonpeptide antagonist of the human luteinizing hormone-releasing hormone (LHRH) receptor. J Med Chem 41: 4190–4195
Buchter D et al. (1999) Clinical trial of transdermal testosterone and oral levonorgestrel for male contraception. J Clin Endocrinol Metab 84: 1244–1249
Hair WM et al. (2001) A novel male contraceptive pill–patch combination: oral desogestrel and transdermal testosterone in the suppression of spermatogenesis in normal men. J Clin Endocrinol Metab 86: 5201–5209
Gonzalo IT et al. (2002) Levonorgestrel implants (Norplant II) for male contraception clinical trials: combination with transdermal and injectable testosterone. J Clin Endocrinol Metab 87: 3562–3572
Guerin JF and Rollet J (1988) Inhibition of spermatogenesis in men using various combinations of oral progestagens and percutaneous or oral androgens. Int J Androl 11: 187–199
Pollanen P et al. (2001) Combination of subcutaneous levonorgestrel implants and transdermal dihydrotestosterone gel for male hormonal contraception. Int J Androl 24: 369–380
Steidle C et al. (2003) AA2500 testosterone gel normalizes androgen levels in aging males with improvements in body composition and sexual function. J Clin Endocrinol Metab 88: 2673–2681
Rosen J and Negro-Vilar A (2002) Novel, non-steroidal, selective androgen receptor modulators (SARMs) with anabolic activity in bone and muscle and improved safety profile. J Musculoskelet Neuronal Interact 2: 222–224
Chen J et al. (2005) A selective androgen receptor modulator for hormonal male contraception. J Pharmacol Exp Ther 213: 546–553
Amory JK and Bremner WJ (2005) Oral testosterone in oil plus dutasteride: a pharmacokinetic study in men. J Clin Endocrinol Metab 90: 2610–2617
Wallace EM et al. (1993) Comparison between testosterone enanthate-induced azoospermia and oligoazoospermia in a male contraceptive study I: plasma luteinizing hormone, follicle stimulating hormone, testosterone, estradiol and inhibin concentrations. J Clin Endocrinol Metab 77: 290–293
Amory JK et al. (2001) Daily testosterone and gonadotropin levels are similar in azoospermic and nonazoospermic normal men administered weekly testosterone: implications for male contraceptive development. J Androl 2001 22: 1053–1060
McLachlan RI et al. (2004) Relationship between serum gonadotropins and spermatogenic suppression in men undergoing steroidal contraceptive treatment. J Clin Endocrinol Metab 89: 142–149
Anderson RA et al. (1996) Comparison between testosterone enanthate-induced azoospermia and oligozoospermia in a male contraceptive study. III. Higher 5α-reductase activity in oligozoospermic men administered supraphysiological doses of testosterone. J Clin Endocrinol Metab 81: 902–908
McLachlan RI et al. (2002) Effects of testosterone plus medroxyprogesterone acetate on semen quality, reproductive hormones, and germ cell populations in normal young men. J Clin Endocrinol Metab 87: 546–556
McLachlan RI et al. (2000) Efficacy and acceptability of testosterone implants, alone or in combination with a 5α-reductase inhibitor, for male hormonal contraception. Contraception 62: 73–78
Kinniburgh D et al. (2001) Suppression of spermatogenesis with desogestrel and testosterone pellets is not enhanced by addition of finasteride. J Androl 22: 88–95
Zhang FP et al. (2003) The low gonadotropin-independent constitutive production of testicular testosterone is sufficient to maintain spermatogenesis. Proc Natl Acad Sci USA 100: 13692–13697
Meriggiola MC et al. (2002) Higher testosterone dose impairs sperm suppression induced by a combined androgen–progestin regimen. J Androl 23: 684–690
Yu B and Handelsman DJ (2001) Pharmacogenetic polymorphisms of the AR and metabolism and susceptibility to hormone-induced azoospermia. J Clin Endocrinol Metab 86: 4406–4411
Eckardstein et al. (2002) CAG repeat length in the androgen receptor gene and gonadotrophin suppression influence the effectiveness of hormonal male contraception. Clin Endocrinol (Oxf) 57: 647–655
Acknowledgements
JK Amory is supported, in part, by the National Institute of Child Health and Human Development, a division of the National Institutes of Health, by grant 1K23 HD45386-10A1, and has research funding from Schering AG and GlaxoSmithKline. WJ Bremner and JK Amory are also supported by the National Institute of Child Health and Human Development through cooperative agreements U54-HD-12629 and U54 HD42454 as part of the specialized Cooperative Centers Program in Reproductive Research and the Cooperative Contraceptive Research Centers Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JK Amory has research funding from Schering AG and GlaxoSmithKline.
Rights and permissions
About this article
Cite this article
Amory, J., Page, S. & Bremner, W. Drug Insight: recent advances in male hormonal contraception. Nat Rev Endocrinol 2, 32–41 (2006). https://doi.org/10.1038/ncpendmet0069
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpendmet0069
This article is cited by
-
Improvement of attention deficit/hyperactivity disorder (ADHD) in three adult men during testosterone treatment: a case series
Journal of Medical Case Reports (2022)
-
RISUG® as a male contraceptive: journey from bench to bedside
Basic and Clinical Andrology (2020)
-
Capturing adenylyl cyclases as potential drug targets
Nature Reviews Drug Discovery (2009)